Sunday, Sept. 27, 2015 | 2 a.m.
Gynecologic cancer is a broad term that refers to cancers in the female reproductive system. Thousands of women are diagnosed with these cancers every year, but in many cases the cancers can be successfully treated and even prevented.
“Regular screenings, vaccinations and widespread awareness can help lower gynecologic cancer rates and save women’s lives,” said Dr. Lynn Kowalski, M.D., FACOG, FACS, medical director of the Las Vegas Institute for Robotic Surgery at MountainView Hospital.
Uterine cancer
There are two well-known types of uterine cancer. Endometrial cancer, the more common, is cancer of the uterine lining, while uterine sarcoma, the rarer of the two, develops in the muscular wall of the uterus.
Symptoms: The most telling symptom is abnormal bleeding, particularly postmenopausal bleeding. “When a woman is experiencing bleeding post-menopause, we have to assume it’s cancer until proven otherwise,” Kowalski said. Other symptoms can include pelvic pain and/or abnormal vaginal discharge.
Detection: A biopsy of the uterine lining is required to detect endometrial cancer. It sometimes can be done in a doctor’s office, or it may require dilation and curettage (D and C), which is performed in an operating room. D and C is a procedure to remove uterine tissue.
Risk factors: Obesity, high blood pressure and/or genetics can be risk factors. “In recent years, we’ve been seeing a spike in younger women being diagnosed with uterine cancer due to obesity,” Kowalski said.
Ovarian cancer
Ovarian cancer is fairly uncommon but is the most deadly of all gynecologic cancers.
Symptoms: Ovarian cancer typically causes vague, nonspecific symptoms such as bloating, pelvic and/or abdominal pain, or a lump or mass in the pelvis or abdomen. Because symptoms are hard to pinpoint, it can lead to a delay in diagnosis.
Detection: Suspicion of ovarian cancer typically is raised because of findings on a CT scan or an ultrasound. A diagnosis can be proven only with a biopsy of ovarian tissue.
Risk factors: Some ovarian cancers are linked to a genetic mutation in the BRCA 1 gene or BRCA 2 gene. BRCA 1 and 2 also are linked to breast cancer, as well as melanoma and pancreatic cancer. Other risk factors can be a family history of endometriosis or taking hormone replacement therapy.
Cervical cancer
The cervix is the lower part of the uterus that connects the uterus to the vaginal walls.
Symptoms: Most cervical cancers are detected by an abnormal Pap smear, but bleeding, especially after intercourse, and/or abnormal discharge, also may indicate a problem.
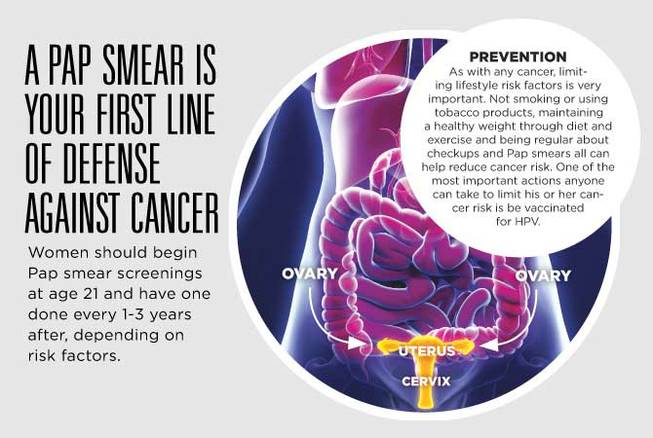
Detection: During Pap smears, cells are scraped from the opening of the cervix and examined for indications of pre-cancer or cancer. An abnormal Pap smear indicates the need for a cervical biopsy. A visible mass on the cervix also may be biopsied, without the need for a Pap smear first. Women should begin Pap smear screenings at age 21 and have one done every 1-3 years after, depending on risk factors.
Risk factors: Cervical cancer almost always is caused by the human papillomavirus (HPV). Women who are carriers of high-risk strains are at greater risk. Smokers also are nearly twice as likely to develop cervical cancer compared with nonsmokers. Other important risk factors include immunosuppressive disorders such as HIV, being a transplant patient or having lupus or rheumatoid arthritis. In addition, the American Cancer Society reports that women younger than 17 during their first full-term pregnancy are almost twice as likely to develop cervical cancer later in life than women who have children at 25 years old or older.
Vaginal and vulvar cancer
Vulvar cancer is cancer of the vulva, which is the outer part of the vagina and includes the vaginal opening, the labia majora (the outer lips of the vagina), the labia minora (the inner lips of the vagina) and the clitoris.
Symptoms: Vulvar cancer is similar to skin cancer; there are many variations that may be cancerous, precancerous or something else entirely. Possible symptoms of vulvar cancer can include a mass, wart-like lumps, open sores, bleeding, itching and/or pain.
Detection: Biopsies are needed to diagnose vulvar cancer.
Risk factors: HPV, age and smoking all are possible risk factors.
•••
Treatment
Depending on the type and stage of gynecologic cancer, surgery, radiation and/or chemotherapy may be necessary. “My biggest suggestion for patients who have been diagnosed with a gynecologic cancer is to see a gynecologic oncologist, not simply a medical oncologist. Seeing a specialist can help improve outcomes greatly,” Kowalski said.
Prevention
As with any cancer, limiting lifestyle risk factors is very important. Not smoking or using tobacco products, maintaining a healthy weight through diet and exercise, and being regular about checkups and Pap smears can all help reduce the cancer risk. One of the most important actions anyone can take to limit their cancer risk is be vaccinated for HPV.
The importance of the HPV vaccine
Because cervical cancer and some vulvar cancers are caused by HPV, the HPV vaccine often is misunderstood as a woman’s preventative measure, but both sexes should be vaccinated. HPV also can cause head and neck cancers, anal cancer and penile cancer. Furthermore, men can be carriers of HPV and spread the virus among their sexual partners. “As with any vaccine, there is a herd effect, so the more people vaccinated, the better,” Kowalski said. “The HPV vaccine can prevent hundreds of thousands of cancers.”
It’s recommended that all children be vaccinated between the ages of 9-12 and before having any sexual contact.

Join the Discussion:
Check this out for a full explanation of our conversion to the LiveFyre commenting system and instructions on how to sign up for an account.
Full comments policy