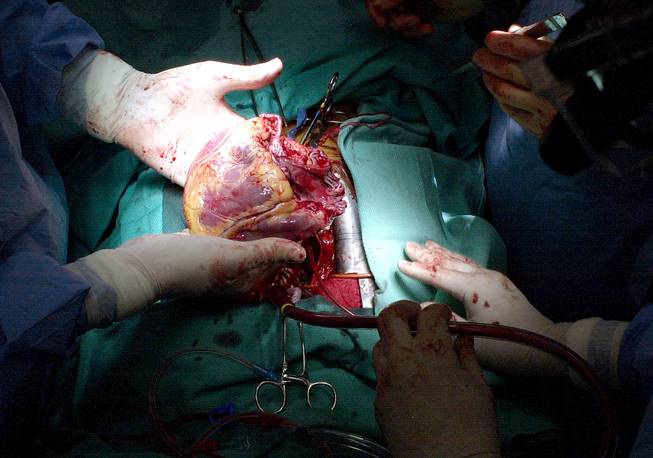
Associated Press file
A doctor holds in his hands a diseased heart which has just been removed from a patient during a heart transplant operation at the Cleveland Clinic in Cleveland.
Monday, Sept. 26, 2016 | 2 a.m.
How to help
Register with the Nevada Donor Network as an organ, eye and/or tissue donor. Visit nvdonor.org, call 855-683-6667 or check yes on the organ-donor box when applying for or renewing a driver’s license, permit, identification card or driver authorization card.
By the numbers:
• 906,596: People registered statewide as donors
• 120,000: Approximate number of people on the national transplant list. Among them, almost 2,000 are children, two-thirds are older than 50 and about 58 percent are minorities.
• 22: Average number of people who die daily waiting for an organ transplant.
• 562: Number of people waiting for an organ transplant in Nevada. Among them are needed: 11 lungs, 103 livers, 1 intestine, 416 kidneys, 3 pancreases, 26 hearts and 8 kidney/pancreas
In July 2015, doctors from Penn Medicine and Children’s Hospital of Philadelphia transplanted two hands and forearms onto an 8-year-old boy in a first-of-its-kind surgery. Only 25 hand transplants have been done worldwide, and Zion Harvey was the first child to undergo the procedure.
It was a success. Weeks later, Zion could wiggle his new hands, which doctors expect will grow with him.
Organ and tissue transplants have come a long way since 1954, when surgeons first transferred an organ from one person to another — a kidney shared between twin brothers. Today, an average of
80 people receive organ transplants each day, but every 10 minutes, another person is added to the national waiting list.
What else can be transplanted?
Tissues: bones, tendons, eyes, skin, nerves, heart valves, veins
More recent medical breakthroughs: face, hands, lower legs
How the transplant process works
Transplants of organs or tissues involve removing a body part from one person and placing it in another person to replace damaged or absent materials. Transplantation is often the only treatment for patients with end-stage organ failure.
Organs typically are harvested from a person who recently died, although some organs and tissues can come from live donors. Tissues, such as heart valves, also can be transplanted from animals.
• Step 1: Referral. Every time a patient dies, hospitals are required by federal law to notify their local organ-procurement organization to determine whether the patient is medically suitable for donation.
Medical conditions that can rule out donation include morbid obesity or a cancer diagnosis. Only 3 in 1,000 people die in a manner that allows for organ donation.
• Step 2: Evaluation. Representatives from the organ-procurement organization review the patient’s medical history to determine whether he or she qualifies as a donor.
• Step 3: Authorization. If the person is a suitable donor, the organ-procurement organization checks the local donor registry to see if the person registered as a donor. If the patient is from another state, the organization coordinates with the organ-procurement group in the patient’s home state to determine whether he or she is a registered donor.
Did you know?
One donor can provide up to nine lifesaving organs and many more tissues.
• Step 4: Family discussion. If the person is a registered donor, staffers from the organization discuss the person’s choice with his or her family, outline the process, answer questions and offer support. If the person is not a registered donor, then staffers offer the family the option of organ donation.
• Step 5: Donor care. If donation is authorized, the organization performs a thorough review of the donor’s health and lifestyle. Once a donor is declared dead or in a state of brain death, the organization assumes responsibility for the donor’s body. Fluids and medications are maintained to preserve the organs and tissues. Information and test results are entered into the United Network of Organ Sharing database to generate a list of potential recipients.
Myth
Some people think that if you register as an organ donor, doctors won’t work as hard trying to save you. In fact, your life always comes first. Organ donation is considered only after a person has died.
• Step 6: Finding recipients. The organization receives a list of possible matching recipients from UNOS. The list uses numerical IDs so the identities of potential recipients remain confidential. Staffers then contact hospital transplant centers with information about the organ. The potential recipient’s surgeon can ask questions and decide whether to accept the organ.
• Step 7: Organ recovery. Once all of the donor’s organs have been matched to recipients, the organization coordinates organ-recovery surgery and transportation, if needed. The donor’s body is then transported to a funeral home.
• Step 8: Family support. Staffers from the organization contact the donor’s family and provide general information about the organs that were donated and the recipients who received them. Organizations also typically provide aftercare to grieving families.
Did you know?
Approximately 95 percent of Americans say they favor being a donor, but only 52 percent are registered to donate.
How quickly must organs be harvested and implanted?
For optimal outcomes, donor materials must be utilized as quickly as possible. Just prior to removal, an ice-cold preservation solution is flushed into the organs, and sterile ice is placed in the body cavity to aid in their cooling. All organs except the kidneys are preserved using hypothermia (kidneys are placed on a machine that constantly pumps solution through them, helping surgeons determine their health). Because of rapid tissue deterioration, UNOS distributes organs locally first.
Finding a match
Doctors screen donor organs carefully for many factors, including size, but most importantly to try to reduce the chance of rejection. The body of a recipient can recognize a transplanted organ as foreign, causing the person’s immune system to attack the new organ. Organ recipients typically must take anti-rejection drugs for the remainder of their lives.

Join the Discussion:
Check this out for a full explanation of our conversion to the LiveFyre commenting system and instructions on how to sign up for an account.
Full comments policy