Monday, Feb. 6, 2017 | 2 a.m.
The American Heart Association (AHA) estimates that 44 million women in the U.S. are affected by cardiovascular diseases, and when combined with stroke, these diseases kill an average of 1 woman every 80 seconds. That’s “1 in 3 female deaths annually,” said Vanessa Gastwirth, MD, FACC, at MountainView Hospital.
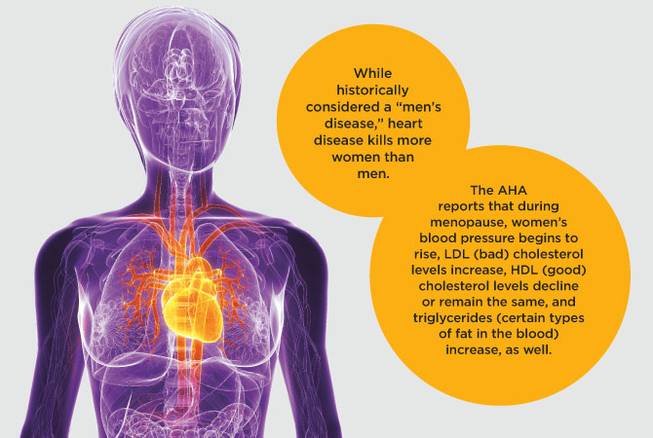
While historically considered a “men’s disease,” heart disease kills more women than men every year. Furthermore, the AHA reports that 90 percent of all women have at least one risk factor for heart disease or stroke.
Common risk factors include age, poor diet, sedentary lifestyle, smoking, genetics and, for some women, hormone levels.
Estrogen can affect your cholesterol levels
Naturally occurring estrogen tends to raise HDL cholesterol levels — the “good” cholesterol that helps carry away artery-clogging LDL cholesterol.
As such, women generally have more HDL cholesterol than men. When estrogen levels peak for women during childbearing years, this HDL provides an extra level of protection from developing heart disease earlier in life.
“Estrogen has favorable effects on health, including an improvement in cholesterol and on the function of blood vessel lining. However, it has adverse side effects as well, such as causing changes in blood proteins that can lead to blood clots, and increased production of inflammatory markers that can lead to vascular disease,” Gastwirth said.
Higher estrogen levels may be protective against some heart diseases, but they are certainly not preventive. Further, menopause causes estrogen levels to drop drastically and can leave postmenopausal women more vulnerable to heart disease.
Menopause and heart disease
Menopause generally occurs in a woman’s late 40s to early 50s, the same age range that heart disease and risk factors begin to develop in both men and women. While postmenopausal women are more prone to heart disease than younger women, researchers aren’t sure how much hormones are at play.
“A postmenopausal state and early natural menopause (occurring in women under 44) is an independent risk factor for cardiovascular disease. However, studies have not proven that menopause itself is a direct cause of cardiovascular disease. The increased rate of cardiovascular disease in postmenopausal women may simply be due to the increased prevalence of other risk factors in older women,” Gastwirth said.
The AHA reports that during menopause, women’s blood pressure begins to rise, LDL (bad) cholesterol levels increase, HDL (good) cholesterol levels decline or remain the same, and triglycerides (certain types of fat in the blood) increase, as well.
For many years, hormone replacement therapy (HRT) used to treat symptoms of menopause was thought to also prevent heart disease, but this has since been disproven. In fact, some studies have indicated that prolonged use of HRT (more than five years) can actually increase the risks of heart disease for women.
While HRT continues to be safely prescribed to women for the purpose of easing significant menopausal symptoms, it no longer is considered a treatment method for heart disease. HRT should be administered conservatively, under a doctor’s close supervision and for no more than five years, or in women older than 65.
Preventing heart disease in women
While there are still many unknowns about heart disease in women — the American College of Cardiology estimates that women comprise 27 percent of participants in all heart-related research studies — we know that maintaining a healthy lifestyle can help slow its development and progression.
“Prevention is extremely important in the management of cardiovascular diseases. Lifestyle modifications such as following a heart-healthy diet, maintaining a normal body weight, regular exercise, not smoking and limiting alcohol consumption can reduce the risk of heart disease and stroke,” Gastwirth said.
She also recommends that women over 20 undergo a cardiovascular risk assessment every three to five years. This assessment should include an evaluation of blood pressure, cholesterol, glucose, smoking habits, activity level and weight.
Birth control and heart disease
Menopause-aged women are not the only ones who need to be concerned about hormone levels and heart health. Hormonal birth control — including pills, patches and rings — can increase a woman’s risk of developing blood clots and cause high blood pressure.
For the average woman, this risk of a blood clot is very small. The National Blood Clot Alliance estimates that annually, 1 in 1,000 women taking birth control pills will develop a dangerous clot, but it’s especially important that these women do not compound the risk by smoking.
“Birth control and smoking should never be combined. Women who do both are at a greatly increased risk of developing cardiovascular disease and blood clots,” Gastwirth said.
Knowing your risk factors can save your life, so talk to your doctor if you’re a smoker and currently taking birth control.

Join the Discussion:
Check this out for a full explanation of our conversion to the LiveFyre commenting system and instructions on how to sign up for an account.
Full comments policy