Monday, Oct. 2, 2017 | 2 a.m.
The Centers for Disease Control and Prevention estimates that as many as 900,000 Americans are affected by deep vein thrombosis (DVT) and pulmonary embolism (PE), and up to 100,000 die from these conditions every year. DVT is an abnormal blood clot that forms within a deep vein, and a pulmonary embolism describes what happens when that blood clot travels into the lungs via the bloodstream.
While common, these conditions can be dangerous, and often develop without warning.
“Pulmonary embolism occurs in 30-40 percent of patients with DVT and sudden cardiac death occurs in 25 percent of those cases,” said Mohi Alkadri, MD, cardiologist at Southern Hills Hospital and Medical Center. Fortunately, DVT can be treated when caught early.
What is a blood clot?
Healthy blood coagulates, or clots, in order to stop bleeding after an injury is sustained. Platelets and plasma proteins inside the blood allow this to happen by forming a solid mass over the broken blood vessel, which can result in a bruise or a scab.
“Under normal circumstances, clots eventually dissolve as part of the healing process,” Alkadri said. However, venous thromboembolism (VTE) occurs when a blood clot forms within an intact vein and does not dissolve naturally.
DVT and PE are two types of VTE. DVT usually occurs within veins of the lower extremities, though it can occur in the upper body, too. A pulmonary embolism is a serious complication of a DVT, wherein the clot gets dislodged from the wall of the vein and travels to the blood vessels of the lungs.
Symptoms and diagnosis
Symptoms of DVT in the lower extremities include leg pain/tenderness, leg swelling, skin that feels warm to the touch and discoloration of the leg/red streaks. These symptoms are caused when blood flow is restricted to the area — the larger the clot, the more severe the symptoms. “Anyone who develops a sudden onset of unilateral calf swelling with localized tenderness, especially if they have other risk factors, should be evaluated for DVT,” Alkadri said.
The symptoms of a pulmonary embolism are much more severe and include shortness of breath, rapid breathing, fast heart rate, chest pain and lightheadedness. If the clot is large enough, it can completely obstruct blood flow into the lungs, causing death or permanent disability.
DVTs can be diagnosed using an ultrasound, and pulmonary embolisms are usually diagnosed using a CT scan. Blood tests may also be used to detect abnormal clotting activity.
Location matters
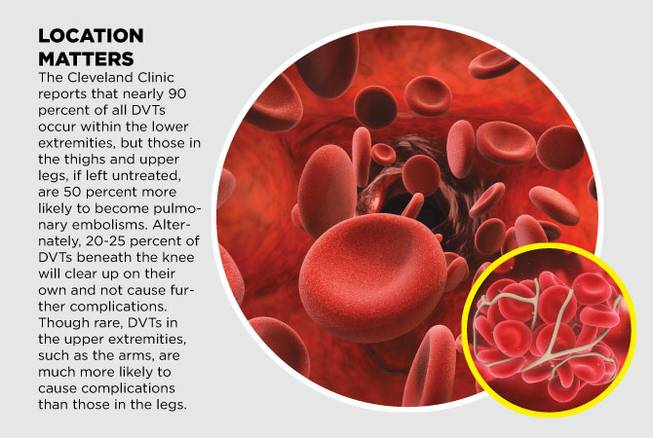
The Cleveland Clinic reports that nearly 90 percent of all DVTs occur within the lower extremities, but those in the thighs and upper legs, if left untreated, are 50 percent more likely to become pulmonary embolisms. Alternately, 20-25 percent of DVTs beneath the knee will clear up on their own and not cause further complications. Though rare, DVTs in the upper extremities, such as the arms, are much more likely to cause complications than those in the legs.
Causes and risk factors
Commonly, DVT occurs when there is a change in the blood flow to the area — possibly caused by surgery or an extended period of immobilization — though some people are more susceptible than others.
“The factors associated with increased risk of DVT formation can be acquired or hereditary,” Alkadri said. “The main acquired risk factors are major surgeries, including hip and knee replacements, and traumas such as hip fractures.”
Hereditary risk factors are often associated with excessive blood-clotting conditions.
Other risk factors include:
• Age, more common in elderly patients
• Weight, more common in overweight patients
• Certain diseases such as cancer and lupus
• Hormones, more common in female patients who are pregnant, on hormone replacement therapy or taking oral contraception
• Being bedridden for more than three days
• History of varicose veins in the legs
Treatment
DVT treatment can vary greatly depending on the patient, their specific risk factors and the location/severity of the clot. Alkadri notes that management options include pharmacological, nonpharmacological and invasive intervention.
Pharmacological treatment methods include blood-thinning medications and anticoagulant drugs (to prevent excessive clotting).
Nonpharmacological treatment methods include compression socks/stockings, intermittent pneumatic compression devices (that cuff around the legs and squeeze to encourage blood flow) and in some cases, inferior vena cava filter placement (which is a small filtering device placed inside the inferior vena cava vein in the abdomen to block the clot from traveling upward into the chest).
Invasive intervention methods involve the surgical removal of blood clots, but these methods are not well established and are offered to only a small selection of patients. “More technology has been investigated in recent years, but additional large-scale studies are needed to confirm the efficacy and cost-effectiveness of these interventions,” Alkadri said.

Join the Discussion:
Check this out for a full explanation of our conversion to the LiveFyre commenting system and instructions on how to sign up for an account.
Full comments policy