Sunday, Nov. 15, 2015 | 2 a.m.
For the 1.6 million Americans living with inflammatory bowel disease, each day can be unpredictable.
As a blanket term for conditions that inflame the digestive tract, inflammatory bowel disease (IBD) includes ulcerative colitis and Crohn’s disease, two disorders with symptoms that manifest in many ways, making research and treatment difficult. “Care of the IBD patient is arguably the most challenging disease state that gastroenterologists encounter,” said Christian Stone, M.D., M.P.H. at Comprehensive Digestive Institute of Nevada and Sunrise Hospital and Medical Center.
As a result, the conditions are incurable, often misunderstood and can have a huge impact on a person’s quality of life.
What causes these conditions, and who is at risk?
Crohn’s disease and ulcerative colitis often are considered autoimmune disorders. That’s because experts believe the illnesses occur when the immune system reacts abnormally, triggering an undue inflammatory response within the body. In essence, the immune system continually attacks a perceived threat, but it’s the immune system’s response that causes the real damage.
Exact risk factors for Crohn’s and colitis are unknown, but family history, environmental factors and ethnicity all may play a role. Scientists do not believe diet causes Crohn’s or colitis, though it can be an exacerbating factor to the existing condition.
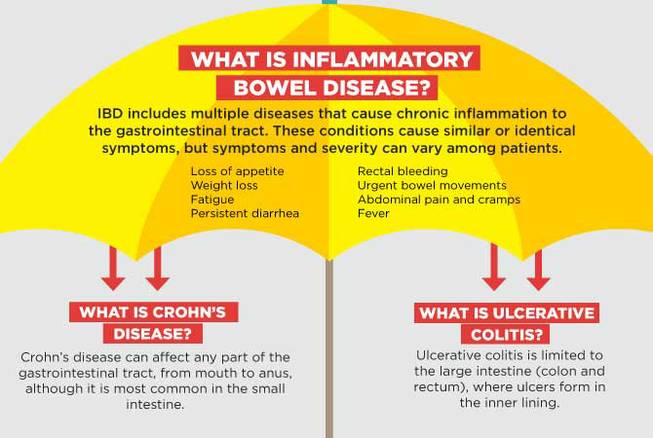
What is inflammatory bowel disease?
IBD includes multiple diseases that cause chronic inflammation to the gastrointestinal tract. These conditions cause similar or identical symptoms, but symptoms and severity can vary among patients.
Symptoms include:
• Loss of appetite
• Weight loss
• Fatigue
• Persistent diarrhea
• Rectal bleeding
• Urgent bowel movements
• Abdominal pain and cramps
• Fever
What is Crohn’s disease?
Crohn’s disease can affect any part of the gastrointestinal tract, from mouth to anus, although it is most common in the small intestine.
Symptoms specific to Crohn’s:
• Mouth sores
• Skin lesions
• Perianal disease (anal inflammation)
What is ulcerative colitis?
Ulcerative colitis is limited to the large intestine (colon and rectum), where ulcers form in the inner lining.
What is the difference between IBD and IBS?
Inflammatory bowel diseases, such as Crohn’s and colitis, are not the same as irritable bowel syndrome or IBS. IBS is a common disorder that affects the colon, causing bloating, cramping, constipation, diarrhea and gas. Unlike Crohn’s and colitis however, IBS does not cause damage or inflammation to the bowel tissue.
Treatment
There are treatment options available for Crohn’s and ulcerative colitis, but there are no cures. “It is imperative that IBD patients seek out a gastroenterologist with expertise in these disorders, given their complexity,” said Stone.
For most patients, treatment is a process of trial and error, as different combinations of medications and lifestyle changes can help manage the disease. Because there are variations of inflammatory bowel disease and because different conditions can present similar symptoms, treating IBD can be difficult. “IBD patients should realize that the main goal of treatment is remission of disease.”
Long-term complications
There are potential long-term complications for people who suffer from Crohn’s or colitis, such as an increased risk of colorectal cancer, malnourishment or a rupture of the bowel.
Among prepubescent children, Crohn’s and colitis also can affect growth and delay development. In addition, it can affect menstruation in women.
Crohn’s disease and celiac disease are often confused
Though they’re not the same, Crohn’s and celiac disease often go hand in hand. They have similar symptoms, and patients with celiac disease may be at higher risk for developing IBD.
Celiac disease is an autoimmune condition triggered by eating gluten. It’s unknown what triggers the immune response in Crohn’s. Patients with celiac disease can successfully manage their symptoms by omitting gluten from their diets.
It is not uncommon for patients with Crohn’s disease also to adopt a gluten-free diet, which for some, can help minimize flare-ups.
How can I support someone with inflammatory bowel disease?
Patients with Crohn’s or colitis often look healthy, despite being sick, and frequently deal with their symptoms privately. Because of the nature of their symptoms, patients may feel embarrassed, ashamed or lonely, and may be hesitant to talk about their pain or discomfort. If you know someone with IBD, consider the following:
• Understand some days are better and some days are worse. People with IBD can feel healthy and happy one day, and be in a great deal of pain the next.
• Listen and be attentive. If they want to discuss their disease, let them. Listen and comfort them if that’s what they need.
• Be understanding about dietary restrictions. A person with IBD may not want to, or be able to, eat at certain restaurants.
• Respect their privacy. People with IBD may not want to discuss their experiences with the disease in detail or at all.
When are symptoms worst?
Crohn’s and colitis both tend to flare up at times, then remain relatively dormant. People with severe symptoms, especially of Crohn’s disease, may have flare-ups daily.
Ulcerative colitis tends to be more mild than Crohn’s, but some patients experience severe and frequent symptoms as well. Flare-ups often are caused by diet or stress.

Join the Discussion:
Check this out for a full explanation of our conversion to the LiveFyre commenting system and instructions on how to sign up for an account.
Full comments policy