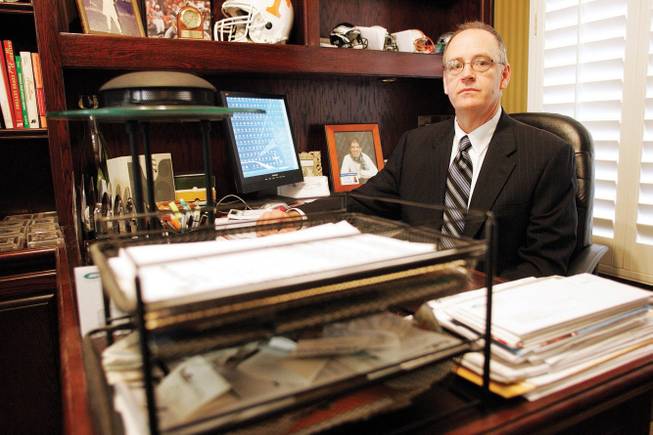
Harry Baut, who was fired as an executive with Behavioral Healthcare Options, brought allegations, now being investigated by Nevada’s Insurance Division, that the company operated for 15 years without needed licenses.
Monday, Aug. 3, 2009 | 2 a.m.
Sun Coverage
Beyond the Sun
Sun Archives
State regulators are investigating whether a subsidiary of Sierra Health Services, the state’s largest health insurance company, operated for up to 15 years without the proper licenses.
The focus of the scrutiny, Behavioral Healthcare Options Inc., is one of several companies under the umbrella of Sierra, which insures about 525,000 Nevadans.
The subsidiary started in 1991 offered specialized mental health and addiction treatment insurance plans, determined benefits for insurance plans and provided other related services.
At issue is whether Behavioral Healthcare Options, from 1991 to 2006, conducted the sorts of insurance transactions that required it to be licensed by the state. Companies that are licensed are required to be bonded and maintain a certain level of capital reserves, among other accountability measures.
The investigation is being conducted by state Insurance Division, which regulates the industry to protect consumers and levies a 3.5 percent tax on insurance premiums collected by the companies. Unlicensed insurers typically face severe discipline by the Insurance Division, including cease and desist orders, penalties and substantial fines.
A former executive at Behavioral Healthcare Options, Harry Baut, triggered the probe, claiming in a letter to state regulators that the subsidiary adjudicated claims and provided insurance for about 15 years without the appropriate state licenses.
Peter O’Neill, spokesman for Sierra and its subsidiaries, denies any wrongdoing on the part of Behavioral Healthcare Options. O’Neill said that Baut is disgruntled after being fired from his job and losing his appeal at an arbitration hearing. The company has always complied with Nevada law, O’Neill said.
Baut, who now consults for companies about insurance plans, filed his complaint in May 2005. He contends the former insurance commissioner, Alice Molasky-Arman, ignored it.
Sierra has been one of Nevada’s most successful companies since it was started in 1972 and today dominates the market. Among its business units are Health Plan of Nevada, the state’s first health maintenance organization, and Southwest Medical Associates, the state’s largest multi-specialty physician group.
UnitedHealth Group, the national insurance behemoth, bought Sierra in 2008. Critics said Molasky-Arman was too accommodating to the deal, which resulted in a near-monopoly in the Las Vegas health insurance market. Baut accuses Molasky-Arman of covering up the fact that Behavioral Healthcare Options operated for years without the proper licenses. Other companies would not be forgiven for such unlawful behavior, he said.
Scott Kipper, who became insurance commissioner in January, has reopened the investigation at Baut’s urging. Kipper’s policy is not to comment on investigations, even to confirm their existence.
Baut came to Behavioral Healthcare Options as director of business development in November 2004, and it didn’t take long before he got into a conflict. He challenged what he characterized as CEO Michael Adam’s foul language around women in the office, and things were tense from there, he said.
Baut was told in late February that his performance was deficient and was instructed to market the company’s services in Arizona, Louisiana, Mississippi and Texas, or risk being fired.
Baut said he discovered the company didn’t have necessary licenses in other states, but that when he told Adams, his concerns were dismissed, exacerbating the conflict between the two men. Baut was fired on April 27, 2005.
Nevada law requires licensed insurance brokers such as Baut to report violations of the insurance code to the commissioner’s office, and Baut filed a complaint with the state regulators a few days later.
Baut bolsters his case with depositions taken under oath in his arbitration hearing, which he used to argue that he was unjustly fired — and to gather evidence that the company was operating illegally.
A fundamental question regarding licensure is whether the subsidiary was assuming “risk” for its insurance product — meaning it promised to pay for all the health care costs for patients covered by particular plans. The company’s marketing materials describe its products as “at risk.”
“BHO is prepared to enter into agreements assuming full risk for standard or customized behavioral health benefit plans,” the company’s literature said.
Nevada law says that to assume risk, the subsidiary would need a Certificate of Authority from the Insurance Division, which would subject it to accountability. It never had one.
Company spokesman O’Neill said Behavioral Healthcare Options didn’t need the certificate because the parent company, Health Plan of Nevada, assumed risk on behalf of the subsidiary.
“The Insurance Division was aware of this,” O’Neill said. “The proper licensure was in place.” He also said all taxes were paid.
Baut said that Behavioral Healthcare Options’ Web site, marketing proposals, financial documents and contracts did not mention that the parent company assumed the risk. In addition, the subsidiary was marketing its at-risk products outside Nevada where the parent company had no authority to assume risk, he said.
Baut says Sierra’s explanation is akin to a person saying he can drive legally on his father’s driver’s license.
The Insurance Division has seemed inconsistent on whether the subsidiary needed to be licensed.
In 2007, the division’s assistant chief examiner said a deposition in Baut’s arbitration hearing that if Behavioral Healthcare Options was selling insurance, it would need a Certificate of Authority, a form of license.
But a former Insurance Division official told the Sun in 2008 that Behavioral Healthcare Options never needed a Certificate of Authority because Health Plan of Nevada assumed all risk.
Confusing the issue further: Amy Parks, chief insurance counsel for the Insurance Division, says the previous investigation concluded the subsidiary was not offering an at-risk insurance product — even though the company’s own literature at the time said it did.
Also at issue is the question of whether the subsidiary was acting as a “third party administrator” by adjudicating claims on behalf of other companies — a role that would require a separate license. The company’s marketing materials said it had “full capacity to adjudicate claims.”
But Behavioral Healthcare Options operated without a third party administrator license until 2006.
O’Neill, the company spokesman, said the company got the license after performing a legal review of the services it had been providing for 15 years. The review determined that certain services “could be construed as being similar” to third party administrator services, O’Neill said.
Baut filed his complaint in 2005, but Molasky-Arman’s office did not investigate it until 2007, by which time the subsidiary had obtained its third party administrator license. By then it had also stopped offering its at-risk insurance products — which negated the need for a Certificate of Authority.
Parks, the Insurance Division attorney, said the investigation was closed within six weeks and no fines or penalties were imposed on the company.
But Baut complains that the investigation did not address whether Behavioral Healthcare Options was operating without the proper licenses for the 15 years leading up to 2006, for which, if that is true, it should still be held responsible.

Join the Discussion:
Check this out for a full explanation of our conversion to the LiveFyre commenting system and instructions on how to sign up for an account.
Full comments policy